Migraine is a debilitating condition characterized by a headache of varying intensity, often accompanied by nausea and sensitivity to light and sound. While researchers today still don’t understand the true reason behind this primary headache disorder, many healthcare professionals believe a misalignment of the cervical spine can lead to migraine. However, new evidence-based research studies have determined that cervical disc herniation, a health issue associated with the intervertebral discs of the upper spine, may also cause head pain. The purpose of the following article is to educate patients and help them understand the source of their symptoms as well as to demonstrate several types of treatment effective for migraine and cervical disc herniation.
Contents
Manual Therapies for Primary Chronic Headaches: a Systematic Review of Randomized Controlled Trials
Abstract
This is to our knowledge the first systematic review regarding the efficacy of manual therapy randomized clinical trials (RCT) for primary chronic headaches. A comprehensive English literature search on CINHAL, Cochrane, Medline, Ovid and PubMed identified 6 RCTs all investigating chronic tension-type headache (CTTH). One study applied massage therapy and five studies applied physiotherapy. Four studies were considered to be of good methodological quality by the PEDro scale. All studies were pragmatic or used no treatment as a control group, and only two studies avoided co-intervention, which may lead to possible bias and makes interpretation of the results more difficult. The RCTs suggest that massage and physiotherapy are effective treatment options in the management of CTTH. One of the RCTs showed that physiotherapy reduced headache frequency and intensity statistical significant better than usual care by the general practitioner. The efficacy of physiotherapy at post-treatment and at 6 months follow-up equals the efficacy of tricyclic antidepressants. Effect size of physiotherapy was up to 0.62. Future manual therapy RCTs are requested addressing the efficacy in chronic migraine with and without medication overuse. Future RCTs on headache should adhere to the International Headache Society�s guidelines for clinical trials, i.e. frequency as primary end-point, while duration and intensity should be secondary end-point, avoid co-intervention, includes sufficient sample size and follow-up period for at least 6 months.
Keywords: Randomized clinical trials, Primary chronic headache, Manual therapies, Massage, Physiotherapy, Chiropractic
Introduction
Primary chronic headaches i.e. chronic migraine (CM), chronic tension-type headache (CTTH) and chronic cluster headache has significant health, economic and social costs. About 3% of the general population suffers from chronic headache with female predominance [1]. The International Classification of Headache Disorders III ? (ICDH-III ?) defines CM as ?15 headache days/month for at least 3 months with features of migraine in ?8 days/month, CTTH is defined as on average ?15 days/month with tension-type headache for at least 3 months, and chronic cluster headache as attacks at least every other day for more than 1 year without remission, or with remissions lasting <1 month [2].
About 80% consult their primary physician for primary chronic headache [3], and pharmacological management is considered first line of treatment. However, the risk is that it may cause overuse of acute headache medication due to frequent headache attacks. 47% of those with primary chronic headache in the general Norwegian population overused acute headache medication [1,4]. Considering the high use of acute medication, both prophylactic medication and non-pharmacological management should therefore be considered in the management [5,6]. Prophylactic medication is used only by 3% in the general Norwegian population, while 52% have tried physiotherapy and 28% have tried chiropractic spinal manipulative therapy [3]. Non-pharmacological management has furthermore the advantage of few and usually minor transient adverse events and no pharmacological interaction/adverse event [7].
Previous systematic reviews have focused on RCTs for tension-type headache, migraine and/or cervicogenic headache, but not on efficacy on primary chronic headache [5,6,8-11]. Manual therapy is a physical treatment used by physiotherapists, chiropractors, osteopaths and other practitioners to treat musculoskeletal pain and disability, and includes massage therapy, joint mobilization and manipulation [12].
This is to our knowledge the first systematic review assessing the efficacy of manual therapy randomized controlled trials (RCT) for primary chronic headache using headache frequency as primary end-point and headache duration and intensity as secondary end-points.
Review
Methods
The English literature search was done on CINHAL, Cochrane, Medline, Ovid and PubMed. Search words were; migraine, chronic migraine, tension-type headache, chronic tension-type headache, cluster headache, chronic cluster headache combined with the words; massage therapy, physiotherapy, spinal mobilization, manipulative therapy, spinal manipulative therapy, osteopathic treatment or chiropractic. We identified studies by a comprehensive computerized search. Relevant reviews were screened for additional relevant RCTs. The selection of articles was performed by the authors. All RCTs written in English using either of the manual therapies for CM, CTTH and/or chronic cluster headache were evaluated. Studies including combined headache types without specific results for CM, CTTH and/or chronic cluster headache were excluded. The review included manual therapy RCTs presenting at least one of the following efficacy parameters; headache frequency, duration and pain intensity for CM, CTTH and/or chronic cluster headache as recommended by the International Headache Society�s clinical trial guidelines [13,14]. Headache frequency is a primary end-point, while duration and pain intensity are secondary end-points. Headache diagnoses were preferentially classified according to the criteria of ICHD-III ? or previous editions [2,15-17]. The methodological quality of the included RCTs was evaluated using the PEDro scale, Table 1[18]. A RCT was considered to be of high quality if the PEDro score was ?6 of a maximum score of 10. The methodological quality of the RCTs was assessed by AC. The PRISMA 2009 checklist was applied for this systematic review. Effect size was calculated when possible. Effect size of 0.2 was regarded as small, 0.5 as medium and 0.8 as large [19].
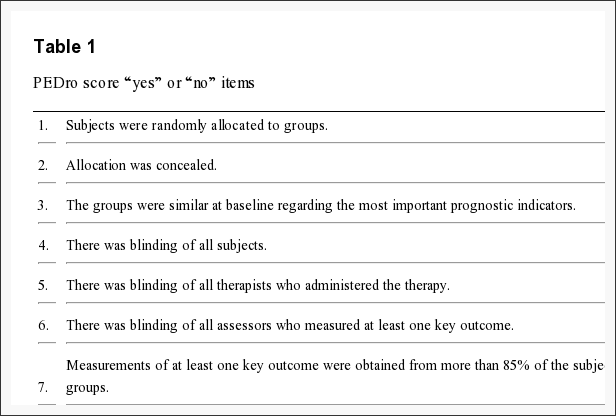
Table 1: PEDro score yes or no items.
This systematic review was executed directly based on the ascertained RCTs available and has not been registered as a review protocol.
Results
The literature search identified six RCTs that met our inclusion criteria. One study applied massage therapy (MT) and five studies applied physiotherapy (PT) [20-25]. All studies assessed CTTH, while no studies assessed CM or chronic cluster headache.
Methodological quality Table 2 shows that the methodological PEDro score of the included RCTs ranged from 1 to 8 points. Four RCTs were considered of good methodological quality, while two RCTs had lower scores.
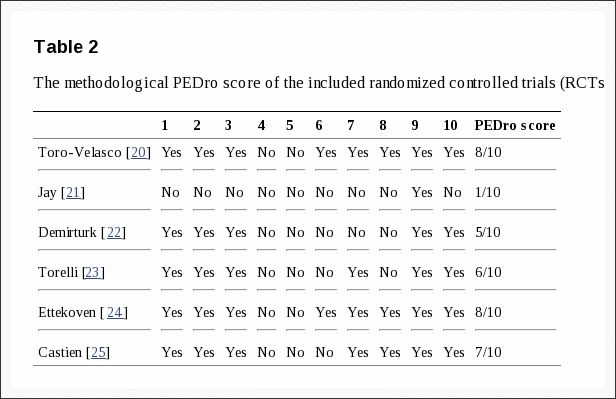
Table 2: The methodological PEDro score of the included randomized controlled trials (RCTs).
Randomized controlled trials (RCT) Table 3 shows the study population, intervention and efficacy of the six RCTs.
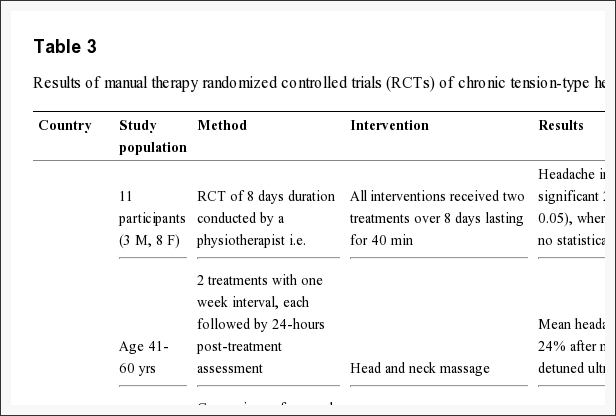
Table 3: Results of manual therapy randomized controlled trials (RCTs) of chronic tension-type headache (CTTH).
Massage therapy A Spanish physiotherapist conducted a 2-armed prospective crossover RCT with pairwise comparisons and blinded outcome measures [20]. The study included participants with CTTH diagnosed by a neurologist. The ICHD-II criteria for CTTH were slightly modified, i.e. pain intensity was defined as ?5 on a 0-10 numeric pain rating scale, and the accompanying symptoms photophobia, phonophobia or mild nausea was not allowed [16]. Primary and secondary end-points were not specified. Results are shown in Table 3.
Physiotherapy An American 3-armed retrospectively RCT had unblinded outcome measures [21]. The diagnostic criteria were ?25 headache days/month for >6 months without associated symptoms nausea, vomiting, photo- and phonophobia, but with tender muscles, i.e. CTTH with pericranial tenderness. Participants with cervicogenic headache or neurological findings were excluded. Primary and secondary end-points were not pre-specified, but headache index, defined here as headache frequency � severity, was the evaluated end-point.
A Turkish study conducted a 2-armed prospective RCT with unblinded outcome measures [22]. The participants were diagnosed with CTTH according to ICHD-I [15]. Participants with mixed headache, neurological and systemic aliment, or participants whom had received physiotherapy within 6 months prior to the study were excluded. Primary end-points was headache index defined as frequency � severity.
A Danish study conducted a 2-armed prospective RCT with blinded outcome measures [23]. Participants were diagnosed CTTH by a neurologist according to the criteria of ICHD-I [15]. Participants with other primary headaches, neuralgia, neurological, systemic or psychiatric disorders or medication overuse defined as >100 analgesic tablets or >2 doses of triptans and ergotamine per month were excluded. The primary end-point was headache frequency, and the secondary end-points were headache duration and intensity. The results shown in Table 3 were not influenced by pericranial muscles tenderness.
A Dutch study conducted a 2-armed prospective, multicentre RCT with blinded outcome measures [24]. Participants were diagnosed with CTTH by a physician according to ICHD-I [15]. Participants with multiple headache types or those whom had received physiotherapy within the last 6 months were excluded. Primary end-points were headache frequency while duration and intensity were secondary end-points.
The 2nd Dutch study conducted a 2-armed prospective pragmatic, multicentre RCT with self-reported primary and secondary end-points, i.e. headache frequency, duration and intensity [25]. Participants were diagnosed by a physician according to the criteria of ICHD-II [16]. Participants with rheumatoid arthritis, suspected malignancy, pregnancy, non-Dutch speaking, those whom had received physiotherapy within the last 2 months, triptan, ergotamine or opiods users were excluded.
Discussion
The current systematic review evaluating the efficacy of manual therapy in RCTs for primary chronic headaches only identified RCTs treating CTTH. Thus, the efficacy of CM and chronic cluster headache could not be evaluated in this review.
Methodological considerations The methodological quality of studies assessing manual therapies for headache disorders are frequently being criticised for being too low. Occasionally rightly so, but often do the methodological design prevent manual therapy studies from reaching what is considered gold standard in pharmacological RCTs. For instance, a placebo treatment is difficult to establish while the investigator cannot be blinded for its applied intervention. The average score of the included studies was 5.8 (SD 2.6) points and four studies were considered of good quality. All RCTs failed to include sample size ?50 in the smallest group. Sufficient sample size with power calculation prior is important to confine type 2 errors. Three studies did not state primary and secondary end-points, which confound effect-size calculation, and risk of type 2 errors inferred from multiple measures [20-22]. Conducting a manual therapy RCT is both time and cost consuming, while blinding often is difficult as there is no single validated standardized sham-treatment which can be used as a control group to this date. Thus, all of the included studies were pragmatic or used no treatment as a control group.
Apart from the participants in the retrospective study [21], all participants were diagnosed by a physician or neurologist. A diagnostic interview is the gold standard, while questionnaire and lay interviews are less precise diagnostic tools regarding headache disorders [26].
Co-intervention was only avoided in two studies [22,20]. Two studies performed intention-to-treat analysis which is recommended to protect against odd outcome values and preserve baseline comparability [24,25,27].
Results The massage therapy study included only 11 participants, but the massage group had significantly more reduction in their headache intensity than detuned ultrasound group [20].
54%, 82% and 85% of the participants in three of the physiotherapy RCTs had a ?50% reduction in headache frequency post-treatment [23-25], and the effect was maintained in the two studies that had a 6 months follow-up [24,25]. This is comparable with the 40-70% of participants whom have a similar effect using tricyclic antidepressants [28,29]. The effect of tricyclic also seems to improve over time, i.e. after more than 6 months treatment [29]. However, tricyclic antidepressants have a series of side effects in contrast to physiotherapy, while manual therapy requires more consultations. Two studies assessed headache index defined as headache frequency � intensity [21,22]. Both studies showed a significant improvement post-treatment and at 1 month and 6 months follow-up respectively.
Four of the studies reported 10.1 mean years with headache, thus, the effect observed is likely to be due to the therapeutic effect rather than spontaneous improvement or regression to the mean [21-23,25].
Acute headache medication is frequently used for primary headaches, and if the headache frequency increases, there is an increased risk for medication overuse headache. Increased use of prophylactic medication has thus been suggested in the management for primary chronic headaches [3]. Since manual therapies seems to have a beneficial effect that equals the effect of prophylactic medication [28,29], without the pharmacological side effects, manual therapies should be considered on an equal level as pharmacological management strategies.
Effect size could be calculated in three of the six RCTs. Effect size on headache frequency was up to 0.62, while it was less regarding duration and intensity, while headache index (frequency � intensity) was up to 0.37 (Table 3). Thus, a small to moderate effect size might however, be substantial to the individual, especially considering that nearly daily headache i.e. mean 12/14 days reduced to mean 3/14 days [25], which equals ?75% reduction in headache frequency. Usually a ?50% reduction is traditionally used in pain trails, but considering the fact that CTTH is difficult to treat, some investigators operate with ?30% improvement of primary efficacy parameter compared with placebo [30].
Limitations The present study might have possible biases. One of them being publication bias as the authors made no attempt to identify unpublished RCTs. Although we did perform a comprehensive search, we acknowledge it is possible to miss a single or few RCT, especially non-English RCT.
Conclusion
Manual therapy has an efficacy in the management of CTTH that equals prophylactic medication with tricyclic antidepressant. At present no manual therapy studies exist for chronic migraine or chronic cluster headache. Future manual therapy RCTs on primary chronic headache should adhere to the recommendation of the International Headache Society, i.e. primary end point is headache frequency and secondary end-points are duration and intensity. Future manual therapy studies on CM with and without medication overuse is also warranted, since such studies do not exist today.
Competing Interests
The authors declare that they have no competing interests.
Authors� Contributions
AC prepared the initial draft and performed the methodological assessment of the included studies. MBR had the original idea of the study, planned the overall design and revised the drafted manuscript. Both authors have read and approved the final manuscript.
Authors� Information
Aleksander Chaibi is a BPT, MChiro, PhD student and Michael Bj�rn Russell is a professor, MD, PhD, DrMedSci.
Acknowledgements
Akershus University Hospital, Norway, kindly provided research facilities.
Funding: The study received funding from Extrastiftelsen, the Norwegian Chiropractic Association in Norway and University of Oslo.
Dr. Alex Jimenez’s Insight
Cervical disc herniation is a common condition which occurs when an intervertebral disc in the neck, or cervical spine, ruptures and its soft, gel-like center leaks out into the spinal canal, adding pressure to the nerve roots. Cervical herniated discs can cause symptoms of pain, numbness and weakness in the neck, shoulders, chest, arms and hands as well as radiating symptoms along the lower extremities. Migraine can also be a symptoms associated with herniated discs in the neck. As we age, the intervertebral discs naturally begin to degenerate, making them more susceptible to damage or injury. Common causes of cervical disc herniation include wear and tear, repetitive movements, improper lifting, injury, obesity and genetics.
Long Term Follow-Up of Cervical Intervertebral Disc Herniation in Patients Treated with Integrated Complementary and Alternative Medicine: a Prospective Case Series Observational Study
Abstract
Background
Symptomatic cervical intervertebral disc herniation (IDH) presenting as neck pain accompanied by arm pain is a common affliction whose prevalence continues to rise, and is a frequent reason for integrative inpatient care using complementary and alternative medicine (CAM) in Korea. However, studies on its long term effects are scarce.
Methods
A total 165 patients with cervical IDH admitted between January 2011 and September 2014 to a hospital that provides conventional and Korean medicine integrative treatment with CAM as the main modality were observed in a prospective observational study. Patients underwent CAM treatment administered by Korean medicine doctors (KMDs) in accordance with a predetermined protocol for the length of hospital stay, and additional conventional treatment by medical doctors (MDs) as referred by KMDs. Short term outcomes were assessed at discharge and long term follow-ups were conducted through phone interviews after discharge. Numeric rating scale (NRS) of neck and radiating arm pain, neck disability index (NDI), 5-point patient global impression of change (PGIC), and factors influencing long term satisfaction rates in PGIC were assessed.
Results
Of 165 patients who received inpatient treatment 20.8?�?11.2 days, 117 completed the long term follow-up up at 625.36?�?196.7 days post-admission. Difference in NRS between admission and discharge in the long term follow-up group (n?=?117) was 2.71 (95 % CI, 2.33, 3.09) for neck pain, 2.33 (95 % CI, 1.9, 2.77) for arm pain, and that of NDI 14.6 (95 % CI, 11.89, 17.32), and corresponding scores in the non-long term follow-up group (n?=?48) were 2.83 (95 % CI, 2.22, 3.45) for neck pain, 2.48 (95 % CI, 1.84, 3.12) for arm pain, and that of NDI was 14.86 (95 % CI, 10.41, 19.3). Difference in long term NRS of neck pain and arm pain from baseline was 3.15 (95 % CI, 2.67, 3.64), and 2.64 (95 % CI, 1.99, 3.29), respectively. PGIC was reported to be �satisfactory� or higher in 79.5 % of patients at long term follow-up.
Conclusions
Though the observational nature of this study limits us from drawing a more decisive conclusion, these results suggest that integrative treatment focused on CAM in cervical IDH inpatients may achieve favorable results in pain and functional improvement.
Trial Registration
ClinicalTrials.gov Identifier: NCT02257723. Registered October 2, 2014.
Keywords: Cervical intervertebral disc herniation, Complementary and alternative medicine, Integrative treatment, Inpatient treatment
Background
Neck pain is a common compliant whose point prevalence is estimated at 10�18 %, with lifetime prevalence reaching 30�50 %. Prevalence of neck pain in populations aged 40 or older is approximately 20 % [1, 2]. Neck pain is also related with restricted neck movement [3], and frequently accompanied by headache, dizziness, visual impairment, tinnitus, and autonomic nervous system dysfunction [4, 5]. Frequent concurrent symptoms include upper extremity pain and neurological disorders [6], and neck pain symptoms also persist in many cases leading to work loss due to discomfort [7]. Neck-related disability is generally more serious in patients with radiating pain than pain limited to the neck area [8, 9], and the main characteristic of cervical intervertebral disc herniation (IDH) is arm pain in the region innervated at the herniated disc level and/or compressed nerve root [10, 11].
The range of available treatments for cervical IDH is vast, spanning conservative treatments to various surgical modalities. Conservative treatments include NSAIDs, oral steroids, steroid injections, patient education, rest, Thomas collars, and physical therapy [12�14]. Surgical treatment may be considered when conservative treatment fails. Neuropathy from spinal cord compression is an absolute indication for surgery. Other indications include nerve root compression signs and related motor and sensory loss. Relative indications may involve decreased quality of life due to prolonged chronic pain [15]. While surgical treatment may benefit some patients suffering severe neurological symptoms, most studies on neuropathic pain of the spine state that the long term effects are not significant [16�20]. Although studies on the effect of conservative treatment in cervical IDH patients have occasionally been reported, whether it is effective is yet a matter of controversy, and there is a paucity of studies on the effect of complementary and alternative medicine (CAM) treatment.
According to Benefits by Frequency of Disease data from the 2013 Korean National Health Insurance Statistical Yearbook [21], 5585 patients received treatment for cervical disc disorders for 99,582 days in outpatient care, of which 100,205 days were covered by the National Health Insurance, and medical treatment expenses eligible for reimbursement surmounted to 5,370,217 Korean Won, with 4,004,731 Korean Won reimbursed. Cervical disc disorders was the 12th most frequent reason for admission to Korean medicine hospitals, showing that it is not uncommon to receive inpatient care for cervical IDH.
Such CAM treatments as acupuncture, pharmacopuncture, herbal medicine, and manual therapy are well-sought in Korea to the aim of securing a less invasive, non-surgical method of treatment. Jaseng Hospital of Korean medicine, a Korean medicine hospital accredited by the Korean Ministry of Health and Welfare to specialize in spine disorders, treats over 900,000 spinal disease outpatient cases per year. This hospital manages patients with an integrative system utilizing conventional and Korean medicine, where conventional doctors and Korean medicine doctors (KMDs) cooperate for optimal treatment results. Conventional doctors participate in diagnosis using imaging technology such as X-rays and MRIs, and in treatment by caring for a small percentage of patients potentially in need of more intensive care. KMDs supervise and manage the main treatment of all patients, and decide whether the patient requires additional diagnosis and treatment from a conventional doctor. Cervical IDH patients suffering neck pain or radiating pain unable to receive outpatient treatment are thus provided with concentrated non-surgical integrative treatment during admission.
Despite the widespread use of inpatient treatment for cervical IDH encompassing a number of treatment modalities, studies on its treatment effect in patients admitted for cervical IDH are scarce. An integrative inpatient treatment approach with focus on CAM may not be widely available to patients, and the objective of this study is to introduce and assess the feasibility and long term effect of this integrative treatment model in inpatients with cervical IDH using a practical study design.
Methods
Study Design
This study is a prospective observational study. We observed patients with a main complaint of neck pain or radiating arm pain diagnosed as cervical IDH and admitted from January 2011 to September 2014 at Jaseng Hospital of Korean medicine in Korea which provides integrated conventional and Korean medicine services with CAM as the main modality. The authors conducted a long term follow-up by phone interview during March 2015. Outcome measures covered 5 parts: numeric rating scale (NRS), neck disability index (NDI), patient global impression of change (PGIC), ever-surgery after discharge, and current treatment.
This study is a report on part of a registry collecting prospective data on integrated treatment for musculoskeletal disorder patients (ClinicalTrials.gov Identifier: NCT02257723). The study protocol was approved by the Institutional Review Boards of Jaseng Hospital of Korean medicine. All participants gave written informed consent prior to participation.
Participants
Patients meeting the following criteria were included.
- Admission for treatment of neck pain or radiating arm pain
- Cervical IDH confirmed on MRI
- Diagnosis by KMD that main cause of chief complaint (neck pain or radiating pain) is cervical IDH
Patients meeting the following criteria were excluded.
- Main complaint other than neck pain or radiating pain
- Concomitant musculoskeletal complaint (e.g. low back pain, knee pain)
- Cause of neck pain unrelated to cervical IDH (e.g. spinal tumor, pregnancy, rheumatoid arthritis)
- Refusal to participate in the study or nonagreement to collection and disclosure of personal information for study purposes
KMDs assessed the cause of current neck pain or arm pain symptoms with reference to neurological test results (sensory loss, motor weakness, and tendon reflex) and MRI readings by radiology specialists. Patients who met the proposed inclusion criteria were visited at the inpatient ward on the first day of admission for assessment by a KMD, and followed up using a similar interview and survey process upon discharge. If a patient was admitted multiple times during the study period, only the first admission record was appraised and included.
Interventions
Though the treatment protocol was comprised with most frequented treatments for cervical IDH patients, any and all treatment methods not included in the treatment protocol were allowed and available to all physicians and patients and use of these treatments (type and frequency) were recorded in electronic medical records pragmatically. Conventional treatments such as pain medications and epidural injections (using local anesthetics such as lidocaine, steroids, and anti-adhesion adjuvants) were administered by a conventional rehabilitation specialist through KMD referral. Only non-surgical treatments were allowed during admission.
Complementary and Alternative Medicine Treatment Protocol
Herbal medicine was taken 3 times/day in pill (2 g) and water-based decoction form (120 ml) (Ostericum koreanum, Eucommia ulmoides, Acanthopanax sessiliflorus, Achyranthes bidentata, Psoralea corylifolia, Saposhnikovia divaricata, Cibotium barometz, Lycium chinense, Boschniakia rossica, Cuscuta chinensis, Glycine max, and Atractylodes japonica). These herbs were carefully selected from herbs frequently prescribed for IDH treatment in Traditional Chinese Medicine and Korean Medicine [22] and the prescription was further developed through clinical practice [23]. The main ingredients of the herbal medicine used in this study (Acanthopanax sessiliflorus Seem, Achyranthes japonica Nakai, Saposhnikovia divaricata Schischk, Cibotium barometz J. Smith, Glycine max Merrill, and Eucommia ulmoides Oliver) have been studied in vivo and in vitro as GCSB-5 for their anti-inflammatory [24], and nerve [25] and joint protective effects [26], and clinically for non-inferiority in safety and efficacy compared to Celecoxib in treatment of osteoarthritis [27].
Acupuncture was administered 1�2 sessions/day at cervical Ah-shi points and acupuncture points pertaining to neck pain. Ah-shi point acupuncture refers to acupuncture needling of painful or pathological sites. Ah-shi points do not exactly match tender points or Buding, Tianying points, but generally correspond to points that induce relaxation or pain upon palpation [28].
The pharmacopuncture solution was prepared with ingredients similar to the orally administered herbal medicine (Ostericum koreanum, Eucommia ulmoides, Acanthopanax sessiliflorus, Achyranthes bidentata, Psoralea corylifolia, Saposhnikovia divaricata, Cibotium barometz, Lycium chinense, Boschniakia rossica, Cuscuta chinensis, Glycine max, and Atractylodes japonica) by decocting and freeze drying, then mixing the prepared powder with normal saline and adjusting for acidity and pH. Pharmacopuncture was administered 1 session/day at cervical Hyeopcheok (Huatuo Jiaji, EX B2) and Ah-shi points up to 1 cc using disposable injection needles (CPL, 1 cc, 26G x 1.5 syringe, Shinchang medical co. Korea).
Bee-venom pharmacopuncture was applied if the skin reaction test to bee-venom was negative. Diluted bee-venom solution (mixed with normal saline at a ratio of 1000:1) was injected at 4�5 cervical Hyeopcheok (Huatuo Jiaji, EX B2) and Ah-shi points at the physician�s discretion. Each point was injected with about 0.2 cc up to a total 0.5�1 cc using disposable injection needles (CPL, 1 cc, 26G x 1.5 syringe, Shinchang medical co. Korea)
Chuna spinal manipulation [29, 30], which is a Korean manipulation method that combines conventional manipulation techniques with high-velocity, low amplitude thrusts to joints slightly beyond the passive range of motion, and manual force within the passive range, was conducted 3�5 sessions/week.
Outcome Measures
All outcomes were assessed by KMDs who had received prior training and education. Demographic and health behavior characteristics (sex, age, occupation, smoking, alcohol consumption, and underlying disease) were collected on the first day of admission using short surveys on current pain levels and neurological exams. Follow-ups were conducted at 2 weeks post-admission or upon discharge and after discharge.
NRS [31] uses an 11-point scale to evaluate current neck pain and radiating pain where no pain is indicated by �0�, and the worst pain imaginable by �10�. NRS was assessed at admission, discharge, and long term follow-up. Due to lack of references on minimum clinically important difference (MCID) of neck pain or radiating pain for NRS, MCID for visual analogue scale (VAS) was used for further evaluation of NRS.
The NDI [32] is a 10-item survey that assesses the degree of disability from 0 to 5 in fulfilling daily activities. The total is divided by 50, then multiplied by 100. NDI was assessed at admission and discharge.
PGIC [33] was used to assess patient satisfaction rate of current state after admission. Satisfaction was rated with a 5-point scale ranging from very satisfactory, satisfactory, slightly satisfactory, dissatisfactory, and very dissatisfactory at discharge and long term follow-up.
Participants underwent physical and neurological examination at admission and discharge for objective motor and sensory evaluation of the cervical region. Range of motion (ROM) for neck flexion and extension, distraction, compression, Valsalva, Spurling, Adson�s, and swallowing tests, and upper extremity motor strength and sensory tests and deep tendon reflex tests were performed.
Safety Assessments
All potential adverse events regarding treatment, ranging from skin and local reactions to systemic reactions, and including change or aggravation in pain patterns were carefully observed, recorded and reported during admission. Adverse events associated with bee-venom therapy are known to range from skin reactions to severe immunological responses, and therefore adverse reactions including systemic immunological reactions requiring additional treatment (e.g. antihistaminic agents) were closely monitored. . Blood cell count, liver and renal function tests, and inflammatory activity tests were conducted in all patients at admission, and if there was an abnormal finding requiring follow-up as assessed by KMDs and conventional doctors, relevant markers were rechecked. A total 46 patients were judged to require follow-up at admission by KMDs and conventional doctors and were followed up accordingly during hospital stay, of which 9 patients showed abnormal findings in liver function at admission. Liver function was tracked in these nine patients. Presence of liver injury was also measured to assess possibility of drug-induced liver injury from herbal or conventional medicine intake using a definition of (a) ALT or DB increase of 2� or over the upper limit of normal (ULN) or (b) combined AST, ALP, and TB increase, provided one of them is above 2?�?ULN.
Statistical Methods
All analyses were conducted using statistical package SAS version 9.3 (SAS Institute, Cary, NC, USA), and p?<?0.05 was regarded to be statistically significant. Continuous data is presented as mean and standard deviation, and categorical data as frequency and percent (%). The mean difference in NRS of neck pain, NRS of radiating pain, and NDI between admission (baseline), discharge and long term follow-up was analyzed for significance with 95 % confidence intervals (CIs). Satisfaction rate assessed with a 5-point Likert scale at long term follow-up was recategorized into binary values of satisfactory (very satisfactory, or satisfactory) and dissatisfactory (slightly satisfactory, dissatisfactory, and very dissatisfactory). Multivariable logistic regression analysis was conducted to calculate odds ratios (ORs) and 95 % CIs, and estimate the influence of predictive factors on satisfaction rate. Baseline factors that met p?<?0.10 in univariate analysis were included in the final model with age and sex, and factors were selected using stepwise method (p?<?0.05).
Results
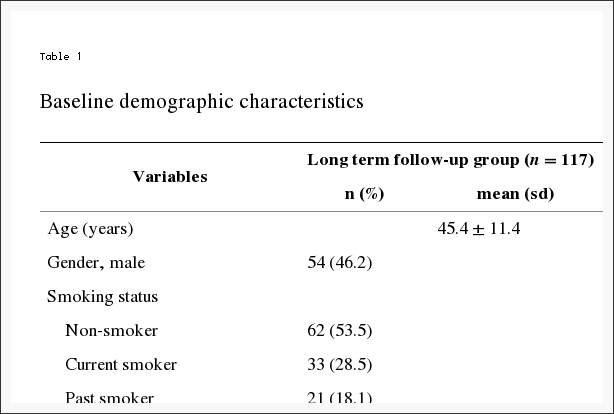
During the study period 784 patients with neck disorders were admitted, and of these, 234 patients were diagnosed with cervical IDH with no other major musculoskeletal complaints. Of the 234 cervical IDH patients, 175 patients had no missing values in NRS and NDI at admission and at 2 weeks post-admission or at discharge (short term follow-up). Ten patients were re-admissions and after inclusion of initial admission data if initial admission was during the study period, 165 patients remained. Long term follow-up assessments were conducted in 117 patients. In the non-long term follow-up group (n?=?48), 23 patients did not answer the phone, 10 refused to participate in the long term follow-up, and 15 had since changed number or had incoming calls barred (Fig. 1). Baseline characteristics by long term follow-up group and non-long term follow-up group are listed in Table 1. Though there were no other marked differences between the 2 groups, 29 patients in the long term follow-up group had been recommended surgery (24.8 %), while only 1 patient in the non-long term follow-up group (0.02 %) had been recommended.
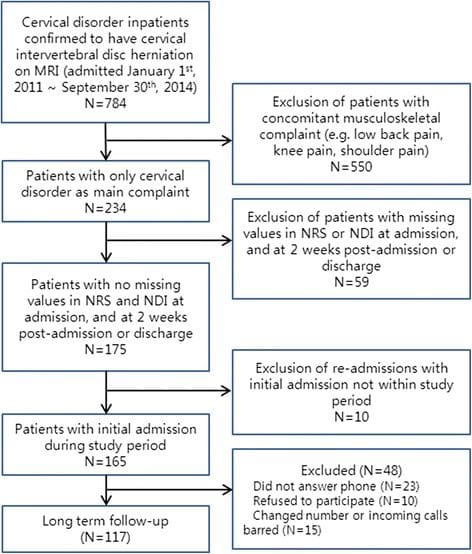
Figure 1: Flow Diagram of the Study
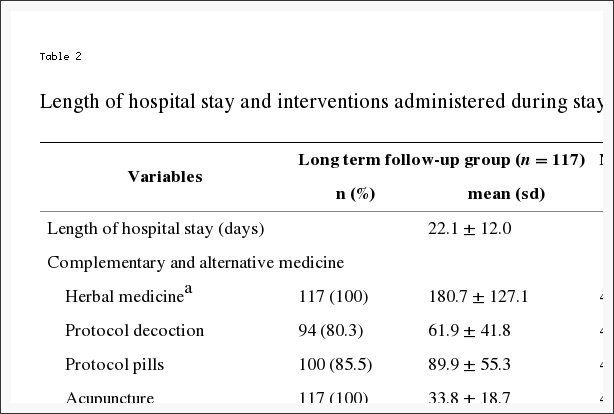
Average length of hospital stay was 20.8?�?11.2 days. The majority of participants received inpatient treatment focused on Korean medicine and CAM. Herbal medicine was taken in accordance with the treatment protocol in decoction form by 81.8 % of patients and in pill form in 86.1 %, and the other patients were prescribed other herbal medicines at the KMD�s discretion. In use of conventional treatments not specified in the CAM treatment protocol, 18.2 % patients took analgesic medications or intramuscular injections an average 2.7?�?2.3 times, and 4.8 % patients were administered 1.6?�?0.5 epidural injections during hospital stay (Table 2). We did not implement restrictions in pharmacological treatment for study purposes, and allowed conventional medicine physicians full freedom to assess and prescribe conventional medicine as the physician deemed necessary for the patient. NSAIDs, antidepressants, and muscle relaxants were the main medicines used, and opioids were administered in the short-term in only 2 patients.
NRS of neck pain, NRS of radiating pain, and NDI all decreased significantly at discharge and at long term follow-up compared to baseline (admission) (Table 3). The major site of pain of neck and radiating arm pain showed a decrease larger than MCID (NRS decrease of 2.5 or larger in neck pain or radiating pain), and NDI scores also improved over the MCID score of 7.5 [34, 35]. Difference in NRS at discharge in the long term follow-up group (n?=?117) was 2.71 (95 % CI, 2.33, 3.09) for neck pain, 2.33 (95 % CI, 1.9, 2.77) for arm pain, and that of NDI, 14.6 (95 % CI, 11.89, 17.32). Difference in NRS at long term follow-up for neck pain and arm pain from baseline was 3.15 (95 % CI, 2.67, 3.64) and 2.64 (95 % CI, 1.99, 3.29), respectively. Difference in NRS at discharge in the non-long term follow-up group (n?=?48) was 2.83 (95 % CI, 2.22, 3.45) for neck pain, 2.48 for arm pain (95 % CI, 1.84, 3.12), and that of NDI was 14.86 (95 % CI, 10.41, 19.3). The between-group difference in effect between admission and discharge in the long term follow-up and non-long term follow-up patients was not significant (NRS of neck pain : p-value?=?0.741; NRS of radiating arm pain: p-value?=?0.646; Neck disability index: p-value?=?0.775).
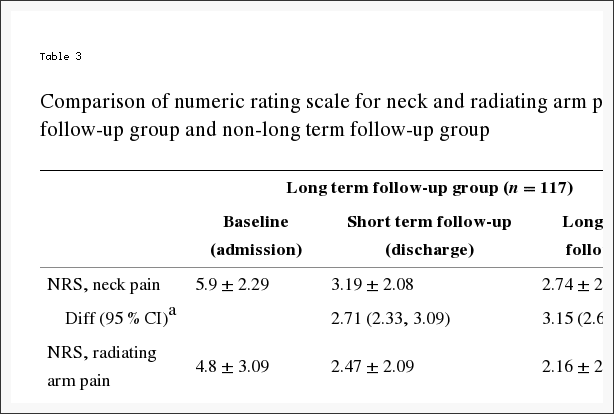
Table 3: Comparison of numeric rating scale for neck and radiating arm pain and neck disability index score in long term follow-up group and non-long term follow-up group.
The average period from admission to long term follow-up was 625.36?�?196.7 days. All 165 patients answered the PGIC at discharge, and of these patients 84.2 % replied that their state was �satisfactory� or higher. A total 117 patients replied to PGIC at long term follow-up, and 79.5 % rated their current state to be �satisfactory� or higher. PGIC was reported to be very satisfactory in 48 patients (41.0 %), satisfactory in 45 (38.5 %), slightly satisfactory in 18 (15.4 %), and dissatisfactory in 6 (5.1 %). Nine patients had undergone surgery (7.6 %), while 21 patients replied that they were currently receiving treatment. Of patients currently under treatment, 10 patients (8.5 %) continued to receive CAM, 12 patients (10.3 %) had selected conventional treatment, and 1 patient was receiving both (Table 4).
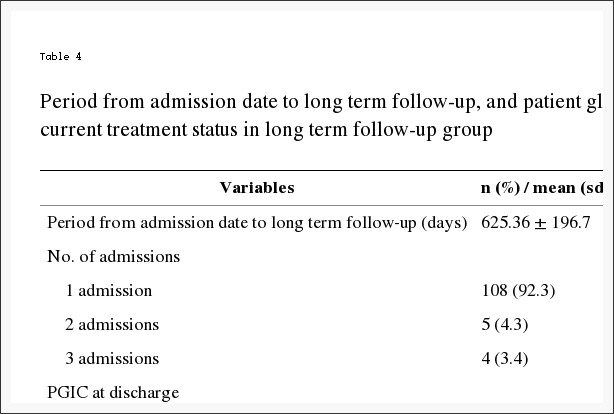
Table 4: Period from admission date to long term follow-up, and patient global impression of change, ever-surgery and current treatment status in long term follow-up group.
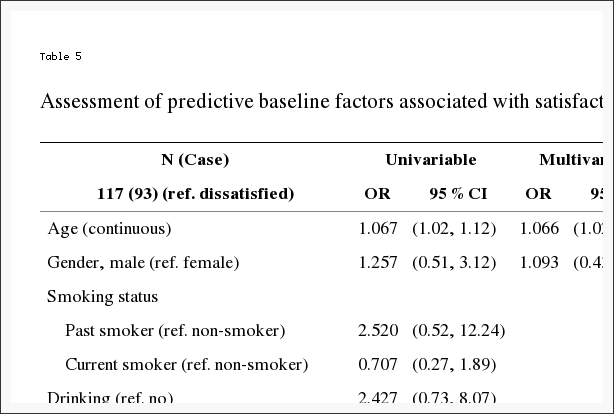
Sex, age, and unilateral radiating pain satisfied p?<?0.10 in univariate analysis of baseline characteristics. Satisfaction rate increased with older age in multivariate analysis. Patients with unilateral radiating arm pain tended to be more satisfied with treatment that those without radiating pain. Also, patients receiving CAM treatment showed higher satisfaction rates than patients receiving no treatment (Table 5).
Liver function was measured in all patients at admission, and nine patients with liver enzyme abnormalities at admission received follow-up blood tests at discharge. Liver enzyme levels returned to normal in 6 patients at discharge, while 2 retained liver enzyme abnormalities, and 1 patient sustained liver injury and on further assessment was diagnosed with active hepatitis showing Hbs antigen positive and Hbs antibody negative. There were no cases of systemic immunological reactions to bee venom pharmacopuncture requiring additional treatment and no other adverse events were reported.
Discussion
These results show that inpatient treatment primarily focused on CAM maintains long term effects of pain relief and functional improvement in cervical IDH patients with neck pain or radiating arm pain. NRS and NDI scores at discharge and at long term follow-up all displayed significant decrease. Also, as statistical significance and clinical significance may differ, we checked for MCID and confirmed that both NRS and NDI scores improved over MCID. MCID has been reported at 2.5 in VAS for neck pain and radiating arm pain, and 7.5 in NDI scores [34, 35]. Average improvement in pain and functionality scales all exceeded MCID, and these results are likely to be reflected in patient satisfaction rate. Out of 165 patients, 128 patients (84.2 %) rated their current state as �satisfactory� or higher at discharge. At long term follow-up, 9 (7.6 %) out of 117 patients were confirmed to have received neck surgery, and most patients showed continued decrease in NRS and NDI. In addition, 96 patients (82.1 %) currently did not receive treatment for neck pain symptoms, and 93 patients (79.5 %) replied their state was �satisfactory� or higher. As comparison of between-group difference in the long term follow-up and non-long term follow-up patients was not designed a priori, this data may be regarded to be a post hoc data analysis. The between-group difference in effect between admission and discharge in the long term follow-up and non-long term follow-up patients was not significant, and in MCID, which could be considered a more clinical measure, the 2 groups produced comparable results.
Despite the fact that all patients underwent intensive Korean medicine treatment for the duration of hospital stay, no adverse events related to treatment were reported, demonstrating the safety of integrative medicine with focus on CAM. The authors had previously conducted a retrospective study to assess safety of herbal medicine and combined intake of herbal and conventional medicine in liver function test results of 6894 inpatients hospitalized at Korean medicine hospitals, and test results of the cervical disc herniation patients included in the present study were also described [36].
A major strength of this study is that it depicts clinical practice and the results reflect treatment as it is actually practiced in Korea in conventional and Korean medicine integrative treatment settings focused on CAM. Protocol treatment was standardized and comprised of interventions whose efficacy has been confirmed in pilot studies and frequently used in clinical practice, but the protocol also allowed for individual tailoring according to patient characteristics and symptoms as seen necessary by KMDs, and the percentage and frequency of these deviations were recorded. The satisfaction rate assessed at discharge not only reflects patient attitude toward treatment effect, but also increased medical costs entailed by inclusion of various treatments. Taking into account that the participants of this study were not patients recruited through advertisements, but patients visiting a Korean medicine hospital from personal choice receiving no economic compensation for study participation, the fact that most patients� satisfaction rate was high is particularly noteworthy. The results of this study contribute to an evidence base for superior efficacy of compositive treatment over individual treatment in patients diagnosed with cervical IDH, and verify feasibility of clinical implementation with consideration for increased compositive treatment costs.
The largest limitation of our study is probably the inherent quality of a prospective observational study lacking a control. We are unable to draw conclusions on whether the suggested CAM integrative treatment is superior to an active control (e.g. surgery, conventional non-surgical intervention) or the natural course of disease. Another limitation is the heterogeneity of the patient groups and treatment composition. Participants were cervical IDH patients of varying symptoms, severity and chronicity whose progress are generally known to differ, and interventions included conventional treatments such as epidural injections or pain medications in some cases. Therefore it would be more accurate to construe these results to be the effect of a conventional and Korean medicine integrative treatment system than that solely of CAM integrative treatment. The compliance rate of 74 % (n?=?175) at 2 weeks post-admission or discharge out of 234 admitted patients is low, especially considering the short follow-up period. This low compliance may be related to patient attitude toward study participation. As participants did not receive direct compensation for trial participation, they may have lacked incentive to continue participation, and the possibility that patients who refused follow-up assessment were dissatisfied with admission treatment should be considered. Long term assessment was conducted by phone interview in 117 patients (70 %) out of 165 baseline participants partly due to lapse in time, which limited the amount and quality of long term information that could be gathered and led to further patient loss from loss of contact.
Another limitation is that we failed to conduct more comprehensive medical evaluations. For example, although participants were diagnosed as disc herniation to be the main pathology based on MRI readings and neurological symptoms by KMDs, additional imaging information such as pathological disc level and severity of herniation were not collected. Also, data on subsequent recurrences, duration of all episodes and whether some were absolutely cured were not included in long term follow-up assessments, limiting multidimensional evaluation. In addition, while these cervical IDH patients required admission for severe neck and arm pain and consequent functional disability, the fact that this was the first attack of neck pain for many may have been cause for more favorable outcome.
However, the influence of long term follow-up compliance may not be confined to availability but potentially be associated with long term treatment effectiveness. As difference in characteristics of long term follow-up and non-long term follow-up patients may be reflected in short-term outcomes assessed at discharge and types and amount of additional conventional treatment, the fact that this study did not consider for these potential effects through additional analyses is a further limitation of this study.
Controversy still surrounds the efficacy of treatments for cervical IDH. While epidural steroid injections are the commonest modality of conservative treatment used in the United States [37] various systematic reviews show that effects are highly variable and not conclusive [38�44]. Two approaches are widely used in epidural injections: interlaminar and transforaminal approaches. The transforaminal approach has been criticized for safety risks [45�50], and though safer than the transforaminal approach, the interlaminar approach also holds potential risks [51�56]. Reports on the efficacy of conventional medicine for neuropathic pain show conflicting results [57�61], and study results on physical therapy are also inconsistent [62�64].
Gebremariam et al. [65] evaluated the efficacy of various cervical IDH treatments in a recent review, and concluded that though the single published study on conservative treatment versus surgery showed that surgery led to better results than conservative treatment, lacking intergroup analysis, there is no evidence supporting that one treatment is more superior. Despite recommendations for initial conservative treatment and management, some patients may select surgery for cervical IDH to the main aim of alleviating radiating pain in neuropathy and preventing progression of neurological damage in myelopathy [66]. Although the evidence base of conventional conservative and surgical treatments for cervical IDH weighing the benefits and harms is somewhat insufficient, the area has been extensively studied, while there is a distinct paucity of correlative studies on CAM.
Manchikanti et al. [67] stated in a 2 year follow-up study comparing epidural injection treatment with lidocaine and a mix of lidocaine and steroids for cervical IDH that NRS in the lidocaine group was 7.9?�?1.0 at baseline, and 3.8?�?1.6 at the 2 year follow-up, while NRS in the lidocaine and steroid group was 7.9?�?0.9 at baseline, and 3.8?�?1.7 at the 2 year follow-up. NDI in the lidocaine group was 29.6?�?5.3 at baseline, and 13.7?�?5.7 at the 2 year follow-up, and NDI in the lidocaine and steroid group was 29.2?�?6.1 at baseline, and 14.3?�?6.9 at the 2 year follow-up. When compared to our study, though improvement in NRS is slightly bigger in the study by Manchikanti et al., that of NDI is similar. The baseline NRS was higher at 7.9 in this previous study, and they did not differentiate between neck pain and radiating pain in NRS assessment.
The 1 year follow-up results comparing conservative treatment and plasma disc decompression (PDD) for contained cervical IDH show that VAS scores decreased 65.73, while NDI decreased 16.7 in the PDD group (n?=?61), and that VAS scores decreased 36.45, and NDI decreased 12.40 in the conservative treatment group (n?=?57) [68]. However, the study subject was limited to contained cervical IDH, the outcome measure for pain was VAS preventing direct comparison, and the follow-up period was shorter than our study.
The model of integrative treatment used at a Korean medicine hospital may be highly disparate from CAM treatment models used in Western countries. Although CAM treatment is gaining widespread popularity in the West, CAM is usually limited to �complementary� rather than �alternative� medicine, and is generally practiced by conventional practitioners as an adjunctive to conventional treatment after education on acupuncture/naturopathy/etc. or through referral to CAM specialists, of whom some do not hold individual practice rights. On the other hand, Korea adopts a dual medical system where KMDs hold practice rights equal to conventional practitioners, and she does not employ a primarily family practice-based medical system, allowing patients the freedom of primary treatment selection of conventional treatment or Korean medicine treatment. The participants of this study were patients visiting and admitted to a Korean medicine hospital for Korean medicine treatment of cervical IDH, and the integrative treatment model implemented at this Korean medicine hospital does not use CAM as a supplementary measure. Therefore, treatment comprised of CAM treatment such as acupuncture, herbal medicine, Chuna manipulation, and bee-venom pharmacopuncture in most patients, and conventional treatment was administered by conventional doctors through referral in a select few. A total 18.2 % of patients received analgesic medications prescriptions 2.7 times over an average admission period of 20.8 days, which is equivalent to 1�2 days worth�s prescription (calculated as 2 times/day), and epidural injections were administered to only 4.8 %, which is low considering that these patients required admission. It can be surmised that the main objective of admission in conservative treatment for most cervical IDH patients is alleviation of pain. The fact that many inpatients displayed significant pain and functional recovery in this study holds relevance for patients considering selecting a Korean medicine hospital for conservative treatment over surgery. Also, patients were confirmed to have maintained their improved state at long term follow-up, and only 9 received surgery out of the 117 patients assessed in the long term.
Patients were divided into 2 groups by satisfaction rate as evaluated at long term follow-up with PGIC, and multivariable logistic regression analysis was conducted on baseline characteristics to assess predictive factors for satisfaction and dissatisfaction. Older age was associated with higher satisfaction rate, and unilateral radiating pain was shown to be related with higher satisfaction rates than no radiating pain. In addition, patients receiving CAM treatment were associated with higher satisfaction rates compared to those not receiving treatment. This could be partly explained by the fact that more older patients may have higher levels of pain and be in more advanced stages of degeneration, resulting in more favorable and satisfactory treatment outcomes. Similarly, patients with unilateral radiating pain suffer neurological symptoms likely to be more severe than those with no radiating pain. In addition, patients continuing to receive CAM treatment may be more favorably predisposed toward CAM, resulting in higher satisfaction rates.
While numerous prospective long term studies have been conducted on injection treatment or surgical procedures, those on CAM treatment and inpatient treatment are few. The results of this study are comparable to the prospective long term results of injection treatment. Few studies have been conducted on admission treatment for patients with a main complaint of cervical IDH, which may be related with the difference in general healthcare systems.
Conclusions
In conclusion, although the observational nature of this study limits us from drawing more decisive conclusions lacking a control, 3 weeks� integrative inpatient treatment mainly comprised of CAM applied to actual clinical settings may result in satisfactory results and pain and functional improvement maintained in the long term in neck pain or radiating arm pain patients diagnosed with cervical IDH.
Acknowledgements
This work was supported by Jaseng Medical Foundation.
Abbreviations
- IDH Intervertebral disc herniation
- CAM Complementary and alternative medicine
- KMD Korean medicine doctor
- NRS Numeric rating scale
- NDI Neck disability index
- PGIC Patient global impression of change
- MCID Minimum clinically important difference
- VAS Visual analogue scale
- ROM Range of motion
- ULN Upper limit of normal
- CI Confidence interval
- OR Odds ratio
- PDD Plasma disc decompression
Footnotes
Competing interests: The authors declare that they have no competing interests.
Authors� contributions: SHB, JWO, JSS, JHL and IHH conceived of the study and drafted the manuscript, and SHB, MRK and IHH wrote the final manuscript. SHB, JWO, YJA and ARC participated in data acquisition, and KBP performed the statistical analysis. YJL, MRK, YJA and IHH contributed to analysis and interpretation of data. SHB, JWO, JSS, JHL, YJL, MRK, YJA, ARC, KBP, BCS, MSL and IHH contributed to the study design and made critical revisions. All of the authors have read and approved the final manuscript.
Contributor information:�Ncbi.nlm.nih.gov/pmc/articles/PMC4744400/
In conclusion, migraine and cervical disc herniation treatment such as manual therapy as well as integrated complementary and alternative medicine may be effective towards the improvement and management of their symptoms. Information referenced from the National Center for Biotechnology Information (NCBI). The above research studies utilized a variety of methods to conclude the final results. Although the findings were shown to be effective migraine and cervical disc herniation treatment, further research studies are required to determine their true efficacy. The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez

Additional Topics: Neck Pain
Neck pain is a common complaint which can result due to a variety of injuries and/or conditions. According to statistics, automobile accident injuries and whiplash injuries are some of the most prevalent causes for neck pain among the general population. During an auto accident, the sudden impact from the incident can cause the head and neck to jolt abruptly back-and-forth in any direction, damaging the complex structures surrounding the cervical spine. Trauma to the tendons and ligaments, as well as that of other tissues in the neck, can cause neck pain and radiating symptoms throughout the human body.

IMPORTANT TOPIC: EXTRA EXTRA: A Healthier You!
OTHER IMPORTANT TOPICS: EXTRA: Sports Injuries? | Vincent Garcia | Patient | El Paso, TX Chiropractor
Blank
References
1. Grande RB, Aaseth K, Gulbrandsen P, Lundqvist C, Russell MB. Prevalence of primary chronic headache in a population-based sample of 30- to 44-year-old persons: the Akershus study of chronic headache. Neuroepidemiology. 2008;30(2):76�83. doi: 10.1159/000116244. [PubMed] [Cross Ref]
2. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629�808. [PubMed]
3. Kristoffersen ES, Grande RB, Aaseth K, Lundqvist C, Russell MB. Management of primary chronic headache in the general population: the Akershus study of chronic headache. J Headache Pain. 2012;13(2):113�120. doi: 10.1007/s10194-011-0391-8. [PMC free article] [PubMed] [Cross Ref]
4. Aaseth K, Grande RB, Kvaerner KJ, Gulbrandsen P, Lundqvist C, Russell MB. Prevalence of secondary chronic headaches in a population-based sample of 30-44-year-old persons: the Akershus study of chronic headache. Cephalalgia. 2008;28(7):705�713. doi: 10.1111/j.1468-2982.2008.01577.x. [PubMed] [Cross Ref]
5. Bronfort G, Nilsson N, Haas M, Evans R, Goldsmith CH, Assendelft WJ, Bouter LM. Non-invasive physical treatments for chronic/recurrent headache. Cochrane Database Syst Rev. 2004;3:1�69. [PubMed]
6. Chaibi A, Tuchin PJ, Russell MB. Manual therapies for migraine: a systematic review. J Headache Pain. 2011;12(2):127�133. doi: 10.1007/s10194-011-0296-6. [PMC free article] [PubMed] [Cross Ref]
7. Carnes D, Mars TS, Mullinger B, Froud R, Underwood M. Adverse events and manual therapy: a systematic review. Man Ther. 2010;15(4):355�363. doi: 10.1016/j.math.2009.12.006. [PubMed] [Cross Ref]
8. Lenssinck ML, Damen L, Verhagen AP, Berger MY, Passchier J, Koes BW. The effectiveness of physiotherapy and manipulation in patients with tension-type headache: a systematic review. Pain. 2004;112(3):381�388. doi: 10.1016/j.pain.2004.09.026. doi:10.1016/j.pain.2004.09.026. [PubMed] [Cross Ref]
9. Fernandez-de-Las-Penas C, Alonso-Blanco C, Cuadrado ML, Miangolarra JC, Barriga FJ, Pareja JA. Are manual therapies effective in reducing pain from tension-type headache: a systematic review. Clin J Pain. 2006;22(3):278�285. doi: 10.1097/01.ajp.0000173017.64741.86. doi:10.1097/01.ajp.0000173017.64741.86. [PubMed] [Cross Ref]
10. Chaibi A, Russell MB. Manual therapies for cervicogenic headache: a systematic review. J Headache Pain. 2012;13(5):351�359. doi: 10.1007/s10194-012-0436-7. [PMC free article] [PubMed] [Cross Ref]
11. Posadzki P, Ernst E. Spinal manipulations for tension-type headaches: a systematic review of randomized controlled trials. Complement Ther Med. 2012;20(4):232�239. doi: 10.1016/j.ctim.2011.12.001. doi:10.1016/j.ctim.2011.12.001. [PubMed] [Cross Ref]
12. French HP, Brennan A, White B, Cusack T. Manual therapy for osteoarthritis of the hip or knee � a systematic review. Man Ther. 2011;16(2):109�117. doi: 10.1016/j.math.2010.10.011. doi:10.1016/j.math.2010.10.011. [PubMed] [Cross Ref]
13. Tfelt-Hansen P, Block G, Dahlof C, Diener HC, Ferrari MD, Goadsby PJ, Guidetti V, Jones B, Lipton RB, Massiou H, Meinert C, Sandrini G, Steiner T, Winter PB. International Headache Society Clinical Trial Subcommittee. Guidelines for controlled trials of drugs in migraine: second edition. Cephalalgia. 2000;20(9):765�786. [PubMed]
14. Silberstein S, Tfelt-Hansen P, Dodick DW, Limmroth V, Lipton RB, Pascual J, Wang SJ. Task Force of the International Headache Society Clinical Trial Subcommittee. Guidelines for controlled trials of prophylactic treatment of chronic migraine in adults. Cephalalgia. 2008;28(5):484�495. doi: 10.1111/j.1468-2982.2008.01555.x. [PubMed] [Cross Ref]
15. Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain: Headache Classification Committee of the International Headache Society. Cephalalgia. 1988;8(suppl 7):1�96. [PubMed]
16. Headache Classification Subcommittee of the International Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9�160. [PubMed]
17. Olesen J, Bousser MG, Diener HC, Dodick D, First M, Goadsby PJ, Gobel H, Lainez MJ, Lance JW, Lipton RB, Nappi G, Sakai F, Schoenen J, Silberstein SD, Steiner TJ. International Headache Society New appendix criteria open for a broader concept of chronic migraine. Cephalalgia. 2006;26(6):742�746. [PubMed]
18. Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro) Aust J Physiother. 2002;48(1):43�49. doi: 10.1016/S0004-9514(14)60281-6. [PubMed] [Cross Ref]
19. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Routledge, USA; 1988.
20. Toro-Velasco C, Arroyo-Morales M, Fernandez-de-las-Penas C, Cleland JA, Barrero-Hernandez FJ. Short-term effects of manual therapy on heart rate variability, mood state, and pressure pain sensitivity in patients with chronic tension-type headache: a pilot study. J Manipulative Physiol Ther. 2009;32(7):527�535. doi: 10.1016/j.jmpt.2009.08.011. [PubMed] [Cross Ref]
21. Jay GW, Brunson J, Branson SJ. The effectiveness of physical therapy in the treatment of chronic daily headaches. Headache. 1989;29(3):156�162. doi: 10.1111/j.1526-4610.1989.hed2903156.x. [PubMed] [Cross Ref]
22. Demirturk F, Akarcali I, Akbayrak T, Citak I, Inan L. Results of two different manual therapy techniques in chronic tension-type headache. Pain Clin. 2002;14(2):121�128. doi: 10.1163/156856902760196333. [Cross Ref]
23. Torelli P, Jensen R, Olesen J. Physiotherapy for tension-type headache: a controlled study. Cephalalgia. 2004;24(1):29�36. doi: 10.1111/j.1468-2982.2004.00633.x. [PubMed] [Cross Ref]
24. Ettekoven VH, Lucas C. Efficacy of physiotherapy including a craniocervical training programme for tension-type headache; a randomized clinical trial. Cephalalgia. 2006;26(8):983�991. doi: 10.1111/j.1468-2982.2006.01163.x. [PubMed] [Cross Ref]
25. Castien RF, Van der Windt DA, Grooten A, Dekker J. Effectiveness of manual therapy for chronic tension-type headache: a pragmatic, randomised, clinical trial. Cephalalgia. 2011;31(2):133�143. doi: 10.1177/0333102410377362. [PubMed] [Cross Ref]
26. Rasmussen BK, Jensen R, Olesen J. Questionnaire versus clinical interview in the diagnosis of headache. Headache. 1991;31(5):290�295. doi: 10.1111/j.1526-4610.1991.hed3105290.x. [PubMed] [Cross Ref]
27. Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869. doi: 10.1136/bmj.c869. [PMC free article] [PubMed] [Cross Ref]
28. Bendtsen L, Jensen R, Olesen J. A non-selective (amitriptyline), but not a selective (citalopram), serotonin reuptake inhibitor is effective in the prophylactic treatment of chronic tension-type headache. J Neurol Neurosurg Psychiatry. 1996;61(3):285�290. doi: 10.1136/jnnp.61.3.285. [PMC free article] [PubMed] [Cross Ref]
29. Jackson JL, Shimeall W, Sessums L, Dezee KJ, Becher D, Diemer M, Berbano E, O�Malley PG. Tricyclic antidepressants and headaches: systematic review and meta-analysis. BMJ. 2010;341:c5222. doi: 10.1136/bmj.c5222. [PMC free article] [PubMed] [Cross Ref]
30. Bendtsen L, Bigal ME, Cerbo R, Diener HC, Holroyd K, Lampl C, Mitsikostas DD, Steiner TJ, Tfelt-Hansen P. Guidelines for controlled trials of drugs in tension-type headache: second edition. Cephalalgia. 2010;30(1):1�16. [PubMed]
Close Accordion
Blank
References
1. Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine (Phila Pa 1976) 1994;19(12):1307�1309. doi: 10.1097/00007632-199406000-00001. [PubMed] [Cross Ref]
2. Brattberg G, Thorslund M, Wikman A. The prevalence of pain in a general population. The results of a postal survey in a county of Sweden. Pain. 1989;37(2):215�222. doi: 10.1016/0304-3959(89)90133-4. [PubMed] [Cross Ref]
3. Hagen KB, Harms-Ringdahl K, Enger NO, Hedenstad R, Morten H. Relationship between subjective neck disorders and cervical spine mobility and motion-related pain in male machine operators. Spine (Phila Pa 1976) 1997;22(13):1501�1507. doi: 10.1097/00007632-199707010-00015. [PubMed] [Cross Ref]
4. Fricton JR, Kroening R, Haley D, Siegert R. Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985;60(6):615�623. doi: 10.1016/0030-4220(85)90364-0. [PubMed] [Cross Ref]
5. Stovner LJ. The nosologic status of the whiplash syndrome: a critical review based on a methodological approach. Spine (Phila Pa 1976) 1996;21(23):2735�2746. doi: 10.1097/00007632-199612010-00006. [PubMed] [Cross Ref]
6. Frank AO, De Souza LH, Frank CA. Neck pain and disability: a cross-sectional survey of the demographic and clinical characteristics of neck pain seen in a rheumatology clinic. Int J Clin Pract. 2005;59(2):173�182. doi: 10.1111/j.1742-1241.2004.00237.x. [PubMed] [Cross Ref]
7. Andersson G. The epidemiology of spinal disorders. In: Frymoyer J, editor. The adult spine: principles and practice. Philadelphia: Lippincott Raven; 1997. pp. 130�141.
8. Rasmussen C, Leboeuf-Yde C, Hestbaek L, Manniche C. Poor outcome in patients with spine-related leg or arm pain who are involved in compensation claims: a prospective study of patients in the secondary care sector. Scand J Rheumatol. 2008;37(6):462�468. doi: 10.1080/03009740802241709. [PubMed] [Cross Ref]
9. Daffner SD, Hilibrand AS, Hanscom BS, Brislin BT, Vaccaro AR, Albert TJ. Impact of neck and arm pain on overall health status. Spine (Phila Pa 1976) 2003;28(17):2030�2035. doi: 10.1097/01.BRS.0000083325.27357.39. [PubMed] [Cross Ref]
10. Abbed KM, Coumans JV. Cervical radiculopathy: pathophysiology, presentation, and clinical evaluation. Neurosurgery. 2007;60(1 Supp1 1):S28�34. [PubMed]
11. Lauerman W, Scherping S, Wiesel S. The spine. In: Wiesel S, Delahay J, editors. Essentials of Orthopedic Surgery. 3. New York: Springer; 2007. pp. 276�332.
12. Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353(4):392�399. doi: 10.1056/NEJMcp043887. [PubMed] [Cross Ref]
13. Hurwitz EL, Carragee EJ, van der Velde G, Carroll LJ, Nordin M, Guzman J, et al. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008;33(4 Suppl):S123�52. doi: 10.1097/BRS.0b013e3181644b1d. [PubMed] [Cross Ref]
14. Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine (Phila Pa 1976) 1996;21(16):1877�1883. doi: 10.1097/00007632-199608150-00008. [PubMed] [Cross Ref]
15. Clark C. The Cervical Spine. 4. Philadelphia: Lippincott Williams & Wilkins; 2005.
16. Engquist M, Lofgren H, Oberg B, Holtz A, Peolsson A, Soderlund A, et al. Surgery versus nonsurgical treatment of cervical radiculopathy: a prospective, randomized study comparing surgery plus physiotherapy with physiotherapy alone with a 2-year follow-up. Spine (Phila Pa 1976) 2013;38(20):1715�1722. [PubMed]
17. Nikolaidis I, Fouyas IP, Sandercock PA, Statham PF: Surgery for cervical radiculopathy or myelopathy. Cochrane Database Syst Rev 2010, (1):CD001466. doi(1):CD001466. [PubMed]
18. Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296(20):2441�2450. doi: 10.1001/jama.296.20.2441. [PMC free article] [PubMed] [Cross Ref]
19. Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356(22):2245�2256. doi: 10.1056/NEJMoa064039. [PubMed] [Cross Ref]
20. Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976) 1983;8(2):131�140. doi: 10.1097/00007632-198303000-00003. [PubMed] [Cross Ref]
21. Kim JD, Son MS. 2013 National Health Insurance Statistical Yearbook. Seoul: Health Insurance Review and Assessment Service and National Health Insurance Service; 2014.
22. Lin XJ, Chen CY. Advances on study of treatment of lumbar disk herniation by Chinese medicinal herbs. Zhongguo Zhong Yao Za Zhi. 2007;32(3):186�191. [PubMed]
23. Stevens L, Duarte H, Park J. Promising implications for integrative medicine for back pain: a profile of a Korean hospital. J Altern Complement Med. 2007;13(5):481�484. doi: 10.1089/acm.2007.6263. [PubMed] [Cross Ref]
24. Chung HJ, Lee HS, Shin JS, Lee SH, Park BM, Youn YS, et al. Modulation of acute and chronic inflammatory processes by a traditional medicine preparation GCSB-5 both in vitro and in vivo animal models. J Ethnopharmacol. 2010;130(3):450�459. doi: 10.1016/j.jep.2010.05.020. [PubMed] [Cross Ref]
25. Kim TH, Yoon SJ, Lee WC, Kim JK, Shin J, Lee S, et al. Protective effect of GCSB-5, an herbal preparation, against peripheral nerve injury in rats. J Ethnopharmacol. 2011;136(2):297�304. doi: 10.1016/j.jep.2011.04.037. [PubMed] [Cross Ref]
26. Kim JK, Park SW, Kang JW, Kim YJ, Lee SY, Shin J, et al. Effect of GCSB-5, a Herbal Formulation, on Monosodium Iodoacetate-Induced Osteoarthritis in Rats. Evid Based Complement Alternat Med. 2012;2012:730907. [PMC free article] [PubMed]
27. Park YG, Ha CW, Han CD, Bin SI, Kim HC, Jung YB, et al. A prospective, randomized, double-blind, multicenter comparative study on the safety and efficacy of Celecoxib and GCSB-5, dried extracts of six herbs, for the treatment of osteoarthritis of knee joint. J Ethnopharmacol. 2013;149(3):816�824. doi: 10.1016/j.jep.2013.08.008. [PubMed] [Cross Ref]
28. Xu RD, Li H. Conception of Ashi points. Zhongguo Zhen Jiu. 2005;25(4):281�283. [PubMed]
29. Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. A meta-analysis of effectiveness relative to other therapies. Ann Intern Med. 2003;138(11):871�881. doi: 10.7326/0003-4819-138-11-200306030-00008. [PubMed] [Cross Ref]
30. Bronfort G, Haas M, Evans R, Kawchuk G, Dagenais S. Evidence-informed management of chronic low back pain with spinal manipulation and mobilization. Spine J. 2008;8(1):213�225. doi: 10.1016/j.spinee.2007.10.023. [PubMed] [Cross Ref]
31. Turk DC, Rudy TE, Sorkin BA. Neglected topics in chronic pain treatment outcome studies: determination of success. Pain. 1993;53(1):3�16. doi: 10.1016/0304-3959(93)90049-U. [PubMed] [Cross Ref]
32. Ponce de Leon S, Lara-Munoz C, Feinstein AR, Wells CK. A comparison of three rating scales for measuring subjective phenomena in clinical research. II. Use of experimentally controlled visual stimuli. Arch Med Res. 2004;35(2):157�162. doi: 10.1016/j.arcmed.2003.07.009. [PubMed] [Cross Ref]
33. Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149�158. doi: 10.1016/S0304-3959(01)00349-9. [PubMed] [Cross Ref]
34. Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J. 2010;10(6):469�474. doi: 10.1016/j.spinee.2010.02.007. [PubMed] [Cross Ref]
35. Parker SL, Godil SS, Shau DN, Mendenhall SK, McGirt MJ. Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine. 2013;18(2):154�160. doi: 10.3171/2012.10.SPINE12312. [PubMed] [Cross Ref]
36. Lee J, Shin JS, Kim MR, Byun JH, Lee SY, Shin YS, et al. Liver enzyme abnormalities in taking traditional herbal medicine in Korea: A retrospective large sample cohort study of musculoskeletal disorder patients. J Ethnopharmacol. 2015;169:407�412. doi: 10.1016/j.jep.2015.04.048. [PubMed] [Cross Ref]
37. Manchikanti L, Falco FJ, Singh V, Pampati V, Parr AT, Benyamin RM, et al. Utilization of interventional techniques in managing chronic pain in the Medicare population: analysis of growth patterns from 2000 to 2011. Pain Physician. 2012;15(6):E969�82. [PubMed]
38. Chou R, Atlas SJ, Stanos SP, Rosenquist RW. Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine (Phila Pa 1976) 2009;34(10):1078�1093. doi: 10.1097/BRS.0b013e3181a103b1. [PubMed] [Cross Ref]
39. Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(Suppl 2):S192�300. doi: 10.1007/s00586-006-1072-1. [PMC free article] [PubMed] [Cross Ref]
40. Staal JB, de Bie RA, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low back pain: an updated Cochrane review. Spine (Phila Pa 1976) 2009;34(1):49�59. doi: 10.1097/BRS.0b013e3181909558. [PubMed] [Cross Ref]
41. Armon C, Argoff CE, Samuels J, Backonja MM, Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology Assessment: use of epidural steroid injections to treat radicular lumbosacral pain: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007;68(10):723�729. doi: 10.1212/01.wnl.0000256734.34238.e7. [PubMed] [Cross Ref]
42. Parr AT, Diwan S, Abdi S. Lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain: a systematic review. Pain Physician. 2009;12(1):163�188. [PubMed]
43. DePalma MJ, Slipman CW. Evidence-informed management of chronic low back pain with epidural steroid injections. Spine J. 2008;8(1):45�55. doi: 10.1016/j.spinee.2007.09.009. [PubMed] [Cross Ref]
44. Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013;38(3):175�200. doi: 10.1097/AAP.0b013e31828ea086. [PubMed] [Cross Ref]
45. Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine (Phila Pa 1976) 2007;32(11):1249�1256. doi: 10.1097/BRS.0b013e318053ec50. [PubMed] [Cross Ref]
46. Rathmell JP, Benzon HT. Transforaminal injection of steroids: should we continue? Reg Anesth Pain Med. 2004;29(5):397�399. [PubMed]
47. Tiso RL, Cutler T, Catania JA, Whalen K. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J. 2004;4(4):468�474. doi: 10.1016/j.spinee.2003.10.007. [PubMed] [Cross Ref]
48. Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001;91(3):397�399. doi: 10.1016/S0304-3959(00)00437-1. [PubMed] [Cross Ref]
49. Wallace MA, Fukui MB, Williams RL, Ku A, Baghai P. Complications of cervical selective nerve root blocks performed with fluoroscopic guidance. AJR Am J Roentgenol. 2007;188(5):1218�1221. doi: 10.2214/AJR.04.1541. [PubMed] [Cross Ref]
50. Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004;100(6):1595�1600. doi: 10.1097/00000542-200406000-00035. [PubMed] [Cross Ref]
51. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012;15(2):131�140. [PubMed]
52. Abbasi A, Malhotra G, Malanga G, Elovic EP, Kahn S. Complications of interlaminar cervical epidural steroid injections: a review of the literature. Spine (Phila Pa 1976) 2007;32(19):2144�2151. doi: 10.1097/BRS.0b013e318145a360. [PubMed] [Cross Ref]
53. Hodges SD, Castleberg RL, Miller T, Ward R, Thornburg C. Cervical epidural steroid injection with intrinsic spinal cord damage. Two case reports. Spine (Phila Pa 1976) 1998;23(19):2137�42. doi: 10.1097/00007632-199810010-00020. [PubMed] [Cross Ref]
54. Kaplan MS, Cunniff J, Cooke J, Collins JG. Intravascular uptake during fluoroscopically guided cervical interlaminar steroid injection at C6-7: a case report. Arch Phys Med Rehabil. 2008;89(3):553�558. doi: 10.1016/j.apmr.2007.08.165. [PubMed] [Cross Ref]
55. McGrath JM, Schaefer MP, Malkamaki DM. Incidence and characteristics of complications from epidural steroid injections. Pain Med. 2011;12(5):726�731. doi: 10.1111/j.1526-4637.2011.01077.x. [PubMed] [Cross Ref]
56. Shanthanna H, Park J. Acute epidural haematoma following epidural steroid injection in a patient with spinal stenosis. Anaesthesia. 2011;66(9):837�839. doi: 10.1111/j.1365-2044.2011.06770.x. [PubMed] [Cross Ref]
57. McCleane G. Does gabapentin have an analgesic effect on background, movement and referred pain? A randomized, double-blind, placebo controlled study. Pain Clinic. 2001;13:103�107. doi: 10.1163/156856901753420945. [Cross Ref]
58. Yildirim K, Sisecioglu M, Karatay S, Erdal A, Levent A, Ugur M, et al. The effectiveness of gabapentin in patients with chronic radiculopathy. Pain Clinic. 2003;15:213�218. doi: 10.1163/156856903767650718. [Cross Ref]
59. Khoromi S, Cui L, Nackers L, Max MB. Morphine, nortriptyline and their combination vs. placebo in patients with chronic lumbar root pain. Pain. 2007;130(1-2):66�75. doi: 10.1016/j.pain.2006.10.029. [PMC free article] [PubMed] [Cross Ref]
60. Khoromi S, Patsalides A, Parada S, Salehi V, Meegan JM, Max MB. Topiramate in chronic lumbar radicular pain. J Pain. 2005;6(12):829�836. doi: 10.1016/j.jpain.2005.08.002. [PubMed] [Cross Ref]
61. Baron R, Freynhagen R, Tolle TR, Cloutier C, Leon T, Murphy TK, et al. The efficacy and safety of pregabalin in the treatment of neuropathic pain associated with chronic lumbosacral radiculopathy. Pain. 2010;150(3):420�427. doi: 10.1016/j.pain.2010.04.013. [PubMed] [Cross Ref]
62. Hahne AJ, Ford JJ, McMeeken JM. Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review. Spine (Phila Pa 1976) 2010;35(11):E488�504. [PubMed]
63. Salt E, Wright C, Kelly S, Dean A. A systematic literature review on the effectiveness of non-invasive therapy for cervicobrachial pain. Man Ther. 2011;16(1):53�65. doi: 10.1016/j.math.2010.09.005. [PubMed] [Cross Ref]
64. Kuijper B, Tans JT, Beelen A, Nollet F, de Visser M. Cervical collar or physiotherapy versus wait and see policy for recent onset cervical radiculopathy: randomised trial. BMJ. 2009;339:b3883. doi: 10.1136/bmj.b3883. [PMC free article] [PubMed] [Cross Ref]
65. Gebremariam L, Koes BW, Peul WC, Huisstede BM. Evaluation of treatment effectiveness for the herniated cervical disc: a systematic review. Spine (Phila Pa 1976) 2012;37(2):E109�18. doi: 10.1097/BRS.0b013e318221b5af. [PubMed] [Cross Ref]
66. Boselie TF, Willems PC, van Mameren H, de Bie RA, Benzel EC, van Santbrink H. Arthroplasty versus fusion in single-level cervical degenerative disc disease: a Cochrane review. Spine (Phila Pa 1976) 2013;38(17):E1096�107. doi: 10.1097/BRS.0b013e3182994a32. [PubMed] [Cross Ref]
67. Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. Cervical epidural injections in chronic discogenic neck pain without disc herniation or radiculitis: preliminary results of a randomized, double-blind, controlled trial. Pain Physician. 2010;13(4):E265�78. [PubMed]
68. Cesaroni A, Nardi PV. Plasma disc decompression for contained cervical disc herniation: a randomized, controlled trial. Eur Spine J. 2010;19(3):477�486. doi: 10.1007/s00586-009-1189-0. [PMC free article] [PubMed] [Cross Ref]
Close Accordion
Professional Scope of Practice *
The information herein on "Migraine and Cervical Disc Herniation Treatment In El Paso, TX Chiropractor" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Our information scope is limited to Chiropractic, musculoskeletal, physical medicines, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez, DC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, RN*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807, New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Florida
Florida License RN License # RN9617241 (Control No. 3558029)
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Dr. Alex Jimenez DC, MSACP, RN* CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card